In January 2026, India confirmed two cases of Nipah virus infection in West Bengal, marking the country’s latest encounter with this highly lethal disease. Both patients are 25‑year‑old healthcare workers linked to the same private hospital near Barasat, where they developed flu‑like symptoms in late December 2025 that quickly progressed to serious neurological complications.
The infections were first flagged as suspected Nipah cases on 11 January by a Viral Research and Diagnostic Laboratory in Kalyani and were confirmed on 13 January by the National Institute of Virology in Pune using RT‑PCR testing. As of 21 January, WHO reported that the male patient is recovering, while the female patient remains in critical condition under intensive care.
Health authorities have traced and monitored 196 close contacts of the two cases, including family members, colleagues, and hospital staff; all contacts have tested negative and remain asymptomatic. Based on current evidence, WHO and other international agencies assess the risk of wider spread of Nipah virus in India 2026 as low at national, regional, and global levels, and they do not recommend any travel or trade restrictions.
What is Nipah virus?
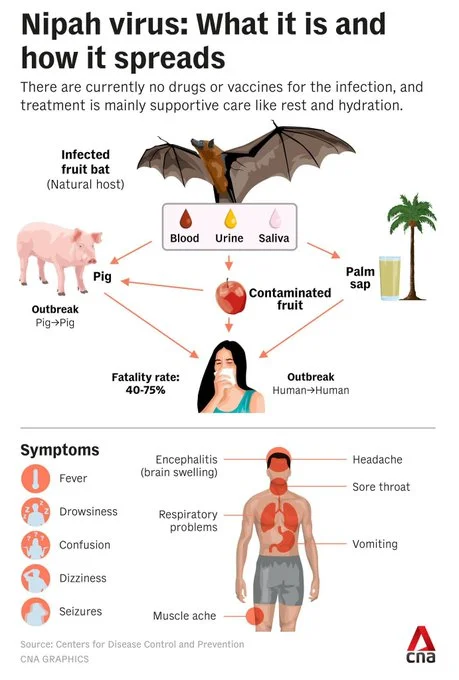
Nipah virus is an emerging zoonotic pathogen that can spread from animals to humans and, in some settings, from human to human. It was first identified in 1999 during an outbreak among pig farmers in Malaysia, where it was named after Kampung Sungai Nipah, the village where the earliest patients lived.
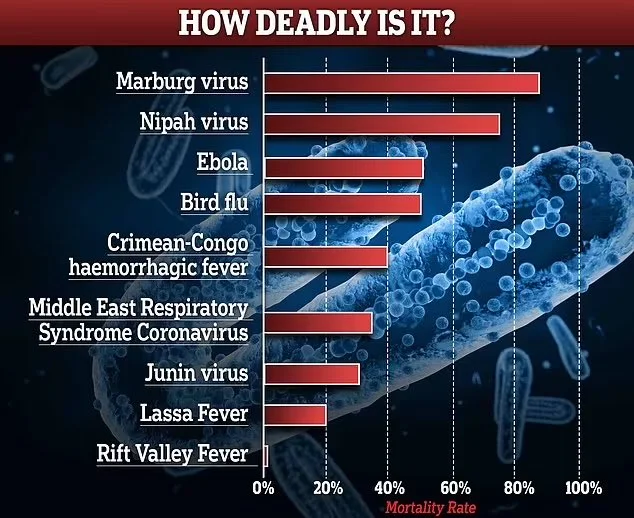
Nipah belongs to the Paramyxoviridae family, the same virus family as measles and mumps, but it behaves very differently. While measles is extremely contagious, Nipah virus is less transmissible but has a far higher fatality rate, often killing 40% to 75% of those infected and, in some Indian outbreaks, exceeding 80%. Because of its ability to cause severe brain and respiratory disease, high mortality, and limited treatment options, WHO classifies Nipah as a priority pathogen and a serious public health threat.
How does Nipah virus spread?
Understanding transmission is crucial to controlling Nipah virus in India 2026. The primary natural reservoir is fruit bats of the genus Pteropus, also known as flying foxes, which are widely found across South and Southeast Asia, including India and Bangladesh. These bats can shed the virus in their saliva, urine, and excreta without appearing sick themselves.
Human infection usually occurs through three main routes:
- Spillover from bats via food: People can get infected by consuming raw date palm sap or fruits contaminated with bat saliva or urine, especially during the sap-harvesting season from December to May.
- Animal-to-human transmission: Domestic animals such as pigs can become intermediate hosts if they ingest material contaminated by infected bats, and then pass the virus to farmers and handlers through close contact with respiratory secretions or bodily fluids.
- Human-to-human spread: Nipah can spread between people through close, unprotected contact with infected patients, particularly in hospitals or households, via respiratory droplets, body fluids, and contaminated surfaces.
Previous outbreaks in India and Bangladesh have shown that family caregivers and healthcare workers are at particular risk when infection prevention and control practices are not strictly followed. The fact that the two Nipah virus in India 2026 cases are nurses reinforces the importance of strong hospital infection control.

Symptoms and complications
The incubation period for Nipah virus typically ranges from 4 to 14 days, although longer periods have occasionally been reported. Most patients initially develop non‑specific, flu‑like symptoms such as fever, headache, muscle pain, vomiting, and sore throat, which can easily be mistaken for more common infections.
In many cases, especially in India and Bangladesh, the illness progresses rapidly to severe neurological disease. Within five to seven days of symptom onset, patients may experience:
- Drowsiness and confusion
- Disorientation or behavior changes
- Seizures
- Encephalitis (inflammation of the brain) and coma
Some individuals develop acute respiratory distress with cough, shortness of breath, or abnormal chest X‑rays, which can complicate management and increase the risk of transmission in crowded settings. Studies show that brain imaging often reveals areas of tissue damage and that changes in the cerebrospinal fluid are consistent with severe viral brain infections.
Even among those who survive Nipah virus infection, long‑term effects are common. Patients may face persistent fatigue, cognitive difficulties, and neurological problems for years, such as personality changes, motor impairment, or recurrent seizures.
How dangerous is Nipah virus?
Nipah virus is considered one of the most dangerous known pathogens. Globally, case fatality rates have ranged from 40% to 75%, depending on the outbreak, medical access, and how quickly cases are identified and isolated. A systematic review of outbreaks from 1994 to 2023 found that India has experienced some of the highest mortality, with estimates above 80% in certain clusters.
Because of its high lethality, potential for human‑to‑human transmission, and absence of widely available vaccines or specific antivirals, Nipah is treated as a biosafety level‑4 agent in laboratories, the highest risk category reserved for viruses like Ebola. Scientists also monitor Nipah closely for any genetic changes that might increase its transmissibility, which is why even a small event like the Nipah virus in India 2026 outbreak attracts global attention.

Diagnosis and treatment
Diagnosing Nipah virus requires specialized laboratory testing. In the current Nipah virus in India 2026 event, confirmation was achieved using RT‑PCR assays on blood or respiratory specimens at the National Institute of Virology. Other tests, such as ELISA to detect antibodies, can help identify recent or past infections during investigations.
At present, there is no licensed vaccine or specific antiviral drug approved for Nipah virus. Clinical management focuses on:
- Supportive care to maintain breathing, blood pressure, and hydration
- Intensive care support for severe respiratory or neurological complications
- Preventing secondary infections and organ failure
The antiviral ribavirin has been studied and may offer limited benefit in some cases, but evidence is mixed and it is not considered a definitive treatment. Several vaccine candidates and experimental therapies are under development, but none are yet available for routine use in outbreaks like Nipah virus in India 2026.

Public health response in India 2026
Following confirmation of the two West Bengal cases, India’s central government deployed a National Joint Outbreak Response Team to assist state authorities. The response has included:
- Intensive contact tracing and daily monitoring of 196 identified contacts
- Enhanced surveillance in hospitals and laboratories in affected districts
- Strict infection prevention and control measures, including PPE for healthcare workers and isolation protocols
- Community risk communication on avoiding raw date palm sap and contact with bats or sick animals
Internationally, several Asian countries including Hong Kong, Malaysia, Singapore, Thailand, and Vietnam have tightened airport health screening for passengers arriving from India. However, WHO, the European Centre for Disease Prevention and Control, and other agencies stress that the likelihood of Nipah virus spreading beyond India is currently low and do not advise travel bans.
How to stay safe during Nipah virus in India 2026
For people living in or traveling to affected areas, simple preventive measures can significantly reduce risk:
- Avoid drinking raw date palm sap and eating fruits that may have been partially eaten or contaminated by bats.
- Limit contact with sick pigs or other animals, and use protective gear if handling them is unavoidable.
- Practice strict hand hygiene, especially after visiting healthcare facilities or caring for sick individuals.
- In hospitals, adhere to mask use, gloves, gowns, and eye protection when treating suspected cases to prevent human‑to‑human spread.
Health authorities emphasize that early detection, rapid isolation, and meticulous infection control are the most powerful tools currently available to contain Nipah virus in India 2026.
As surveillance continues and research progresses, experts hope that future vaccines and antivirals will reduce the heavy toll of this deadly zoonotic disease, especially in countries like India that have historically recorded some of the highest Nipah mortality rates.